Patients with B&J infections, especially chronic osteomyelitis and implant-associated infections often undergo multiple incomplete procedures and receive several courses of empiric antibiotics.
Whereas this practice should be strongly discouraged and every attempt should be made at a tissue diagnosis, fashioning empiric treatment based on the most likely cause is sometimes inevitable when cultures fail to isolate the organism or the patient is clinically unstable.
If ongoing/ recent receipt of empiric antimicrobials, surgery may be deferred for ≥ 2 weeks (antibiotic-free interval), to increase diagnostic yield in a stable patient.
Likely organisms after orthopaedic implant surgery/ PJI based on the interval between surgery and infection
Time of Onset- post implant |
Likely Organisms |
Clinical features |
Very early infection |
Group A Streptococcus |
High fever, shock, bullae, necrosis, gangrene |
Early Infection |
S.aureus |
Fever, inflammation, poor wound healing |
Delayed Infection |
CONS |
Persistent pain, low grade fever, mechanical instability, sinus tract |
Late Infection
|
S. aureus |
-Hematogenous seeding |
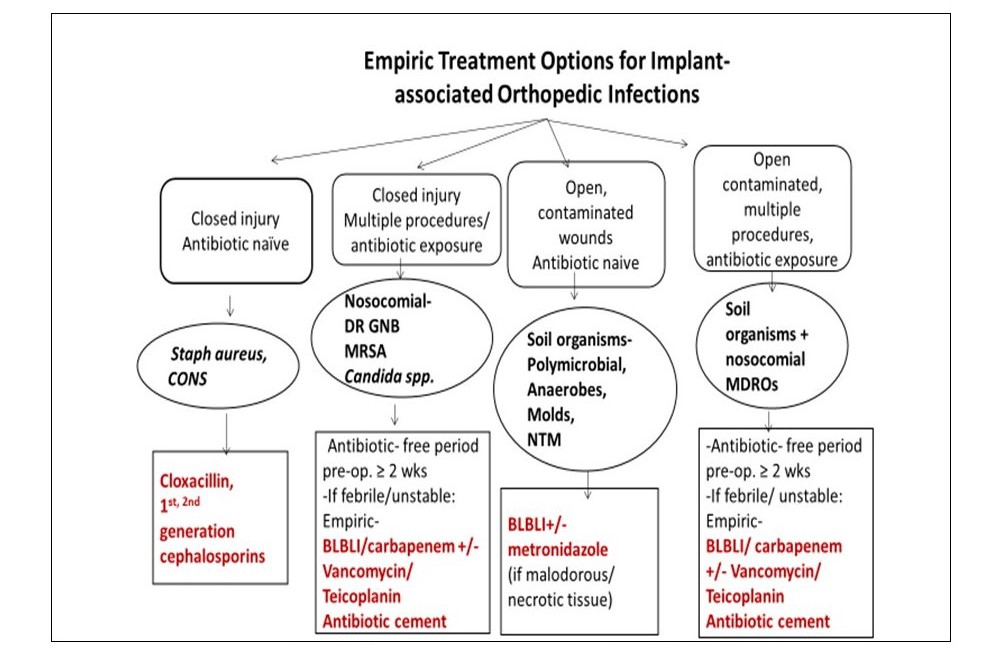
Empiric choices for B&J infections
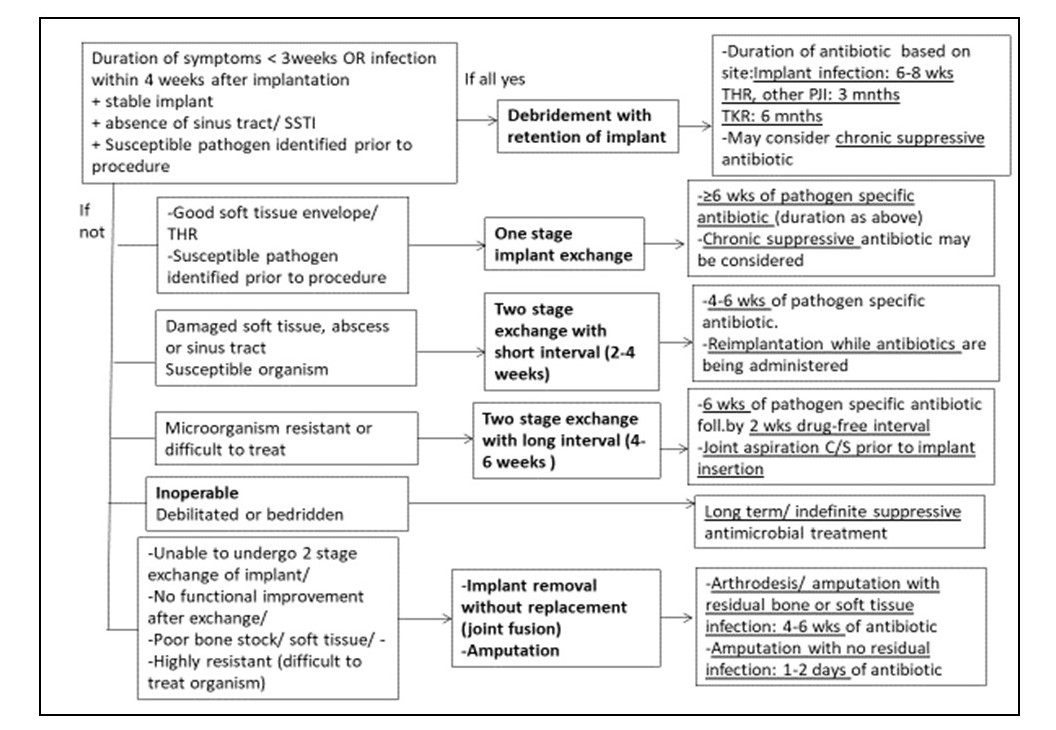
Approach to Prosthetic Joint & Implant-associated Infections